
-
Liver Health: Preventive Measures and Lifestyle Changes to Support Liver Function
posted: Apr. 18, 2024.

-
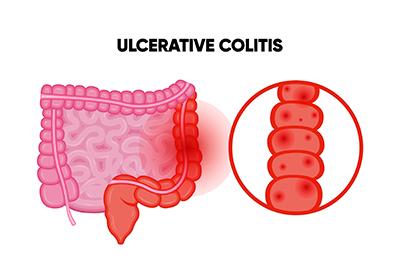
Ulcerative Colitis and Other Digestive Complications
posted: Apr. 01, 2024.
-
Treating Internal Hemorrhoids
posted: Mar. 18, 2024.

-
Three Signs of GERD
posted: Mar. 01, 2024.

-
Are You Dealing With Irritable Bowel Syndrome?
posted: Feb. 16, 2024.

-
Colon Cancer Screening: Understanding Colonoscopies and Other Methods
posted: Feb. 01, 2024.

-
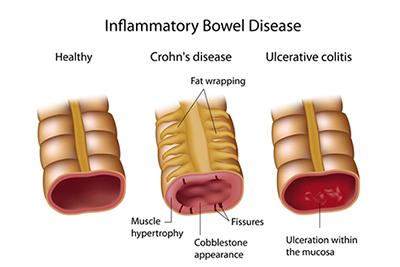
Inflammatory Bowel Disease (IBD): Understanding Crohn's Disease and Ulcerative Colitis
posted: Jan. 16, 2024.
-
What Causes Acid Reflux?
posted: Jan. 01, 2024.

-
Colon Cancer Screening FAQs
posted: Dec. 08, 2023.

-
Don’t Ignore Your Acid Reflux
posted: Dec. 01, 2023.

-
When Is an Endoscopy Needed?
posted: Nov. 10, 2023.

-
The Primary Role of a Gastroenterologist
posted: Nov. 08, 2023.

-
Choosing Us as Your Gastroenterologist
posted: Oct. 10, 2023.

-
Healthy Eating Habits for a Happy Gut
posted: Oct. 05, 2023.

-
What Are the Symptoms of GERD?
posted: Sep. 18, 2023.

Contact Us
Skyline Medical Plaza | Dr. Bailey
Dr. White
3443 Dickerson Pike Skyline Medical Plaza Suite 750 Nashville, TN 37207
(615) 868-1064
Saint Thomas Medical Plaza West | Dr. Bailey
Dr. White
4230 Harding Pike Suite 309 W. Nashville, TN 37205
(615) 329-2141
